|
| Modules in alloFactor |
| |
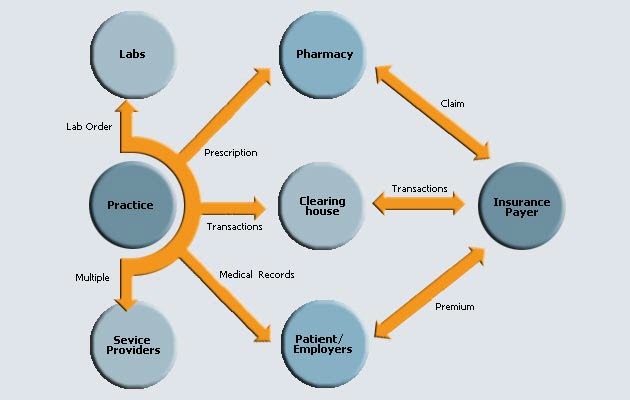
| alloFactor solves all integration issues by acting as the single platform to interface with external entities. No longer does a clinic need to have go to a clearinghouse to submit some claims while faxing a prescription to the pharmacy. alloFactor brings technology to the point of care. |
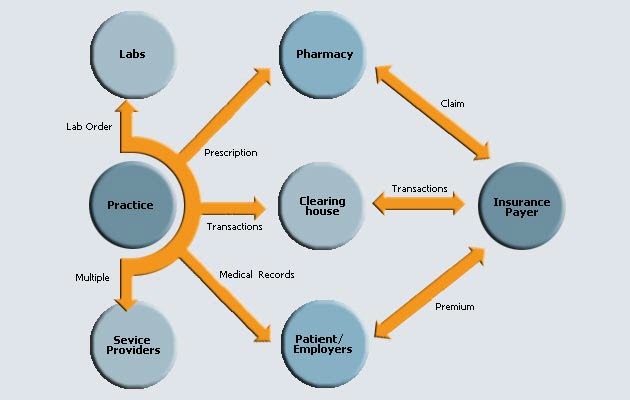 |
| alloFactor is a integrated, workflow based, clinical transaction platform that has modules for each clinical functions built into it so that it works seamlessly to increase productivity, speed and accuracy across the system. A list of systems that are relevant to the proposed solution is discussed below |
Appointment Scheduler
An integrated appointment scheduler helps front-desk manage providers' calendar. User can easily setup patient appointment including recurring appointments. The module also help front-desk track number of cancellations and postponements. |
Registration
Registration module helps the front-desk gather patient information during the initial visit including demographics, employer, guarantor, policyholder and insurance. Insurance companies once setup can be effortlessly mapped to other patients. |
EMR
Electronic Medical Records allows provider to review medical history and record visit related information including Chief Complaint, History of Present Illness, Review of System, Physical Examination, Medication and treatment plan. EMR module has wizards to help generate information using appropriatetemplates with defaults for each field. While EMRs have achieved close to 50% penetration, they seem to be largely restricted to larger practices due to associated costs and skill level requirements. |
Billing
Billing module helps track claims from the patient visit to payment. Once a visit is completed, the claim automatically flows into the billing module. The system eases claim creation and filing of claims electronically or on paper. Payment manager help enter payments either manually or through Auto payment posting. Also it helps scan and store superbills and EOBs. Custom Patient statements may be generated and printed as well. |
Reports
The Reports module helps office manager assess the performance of the clinic. Aging and collection reports are popular amongst. |
Administration
Typically each individual software system will have separate user management. This leads to multiple user id/passwords that are hard to remember. |
Electronic Claim Submission
Electronic claim submission results in faster claim adjudication (typically 3 weeks compared to 6 weeks for paper claims). Electronic claim submission has been adopted by majority of practices as a standard. Few billing software packages have backward integrated clearinghouses while majority of them are clearinghouse neutral allowing practice to choose any clearinghouse to submit claims. Enrolling with clearinghouses is paperwork intensive and most have bad customer service. |
Eligibility Verification
As increasing number of uncovered patients utilize practices, it becomes important to ensure patients coverage. This typically involves manual phone calls to insurance company which could take upto 15 minutes for each patient. Electronic eligibility verifications systems are increasingly becoming popular. |
Auto-payment posting
The exact payment amounts for the treatment rendered will be known only after insurance company processes the claim. When the practice receives the details, the billing team needs to key them in manually into the system to reconcile the charges which is a tedious and error-prone process. Insurance companies have started providing auto-payment posting options which automates the entire payment entry process. |


|